Brain death is a profound and irreversible condition that signifies the complete cessation of all brain activity, and it is clinically recognized as death. The concept of brain death has long been a subject of medical, ethical, and legal discussions, particularly because it challenges our traditional understanding of what constitutes death. One critical aspect that often arises in the context of brain death is the 6-12 minute barrier, a crucial time window that plays a significant role in determining brain death after a cardiac arrest. In this article, we will explore the scientific and medical foundations of the 6-12 minute barrier in brain death, its implications for healthcare practice, and why this window is vital in clinical decision-making.
What is Brain Death?
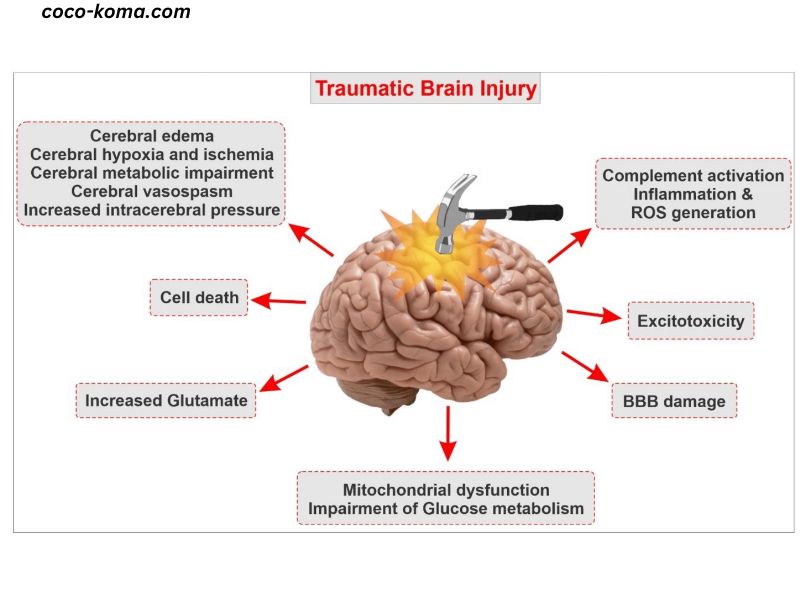
Brain death refers to the complete and irreversible loss of all functions of the brain, including both the brainstem and the cerebrum. It is legally recognized as death in many parts of the world, although the criteria for determining brain death may vary across regions and jurisdictions. Brain death can occur as a result of various causes, such as traumatic brain injury, stroke, or anoxia (lack of oxygen to the brain), often following a cardiac arrest or severe brain injury.
A person who is brain dead may still exhibit signs of bodily function, such as breathing if on a mechanical ventilator, and their heart may continue to beat for a short time. However, the essential hallmark of brain death is that the brain has permanently ceased to function, and there is no chance of recovery.
The Role of Oxygen in Brain Function
The brain, despite accounting for only about 2% of the body’s weight, consumes a disproportionate amount of oxygen—around 20% of the body’s total oxygen supply. Oxygen is essential for maintaining cellular functions and metabolism within the brain, including the generation of energy necessary for neural activity. The brain is particularly vulnerable to oxygen deprivation, and even a few minutes without oxygen can cause significant, irreversible damage.
When the heart stops beating, blood no longer circulates through the body, depriving the brain of oxygen. As a result, brain cells start to die within minutes, leading to irreversible brain injury. The degree of damage depends on how long the brain is deprived of oxygen.
The 6-12 Minute Barrier: What Happens in This Time Window?
The 6-12 minute barrier refers to the critical window of time that occurs after cardiac arrest, during which brain function can be preserved if proper resuscitative measures are taken. After the heart stops, the brain is deprived of oxygen, and irreversible brain damage begins. The brain cells are highly sensitive to the lack of oxygen, and within minutes, the damage becomes increasingly severe.
Key milestones during this critical period include:
- 0-3 Minutes: Within the first few minutes after cardiac arrest, the body can still function to some extent if the heart is rapidly restarted. The brain is highly sensitive during this period, but cellular functions are still somewhat maintained. Medical interventions like CPR (cardiopulmonary resuscitation) or defibrillation during these first few minutes can help restore blood flow to the brain, potentially preventing brain damage.
- 3-6 Minutes: After 3 minutes of oxygen deprivation, the brain begins to experience significant cellular damage. Neurons (brain cells) are particularly vulnerable, as they require a constant supply of oxygen to function. If the brain is not reperfused (re-supplied with oxygenated blood) by this point, the damage becomes more widespread, and the chances of recovery decrease significantly. Medical interventions during this period may still offer some hope for survival, though the prognosis becomes more uncertain.
- 6-12 Minutes: The 6-12 minute window is widely considered the critical period for brain function after cardiac arrest. During this time, the brain suffers substantial and often irreversible damage, leading to the cessation of brain activity. If oxygenated blood is not restored within this window, the brain cells begin to die at an accelerating rate, and the damage is typically too extensive for recovery. This period is crucial for medical practitioners to act quickly and decisively in an attempt to preserve brain function and restore normal circulation. Beyond 12 minutes, the brain is typically considered to be permanently and irreversibly damaged, and brain death is generally confirmed.
Why 6-12 Minutes? Research and clinical observations have shown that brain cells begin to suffer irreversible damage within 4 to 6 minutes of oxygen deprivation. As the period extends into the 6-12 minute range, the likelihood of meaningful brain recovery diminishes sharply. After 12 minutes, the damage is so widespread that even advanced medical interventions are unlikely to result in functional recovery.
Determining Brain Death: Clinical Criteria
Determining brain death is a meticulous process that involves a series of clinical tests and observations. Medical practitioners use specific criteria to confirm the absence of brain activity. These tests include the following:
- Clinical Examination: A thorough neurological examination is conducted to assess the absence of any brain activity. This includes testing for the absence of cranial nerve reflexes, such as pupil response to light, eye movements, and facial muscle responses.
- Absence of Spontaneous Breathing: A brain-dead patient will show no attempt at breathing. The absence of respiratory effort, even when carbon dioxide levels rise in the blood, is a critical indicator of brain death.
- Apnea Test: An apnea test is performed to confirm the lack of respiratory drive. This involves temporarily disconnecting the patient from the ventilator to assess whether they attempt to breathe in response to rising levels of carbon dioxide in the blood.
- Neurological Imaging: Advanced imaging techniques, such as an electroencephalogram (EEG) or cerebral blood flow studies, can be used to confirm the absence of brain activity. An EEG records electrical activity in the brain, and in the case of brain death, it shows a flat line, indicating no electrical activity.
- Confirmatory Tests: In some cases, additional tests may be required to confirm brain death. These tests assess blood flow to the brain and other indicators of brain function. For example, a cerebral angiogram may be performed to detect any residual blood flow to the brain. If no blood flow is detected, brain death is confirmed.
Ethical Considerations of Brain Death
The concept of brain death raises important ethical questions, particularly when it comes to organ donation. In many cases, patients diagnosed as brain dead may still be kept on a ventilator for a time while their organs are considered viable for transplantation. The ethical dilemma involves determining when to discontinue life-sustaining treatment and when it is appropriate to proceed with organ harvesting. These decisions can be particularly challenging for family members who may struggle with the concept of brain death, especially if the body appears to be functioning.
The 6-12 minute barrier also plays a role in the timing of these decisions. If brain death is suspected, medical professionals may need to act quickly to ensure that the patient’s organs remain viable for donation, as organ function deteriorates rapidly once brain death has been confirmed. This underscores the importance of timely interventions within the critical 6-12 minute window.
Conclusion
The 6-12 minute barrier is a crucial time frame in the determination of brain death following cardiac arrest. During this period, the brain is highly vulnerable to oxygen deprivation, and irreversible damage begins to occur as early as the 4-minute mark. By the time the 6-12 minute barrier is reached, the damage to the brain becomes widespread, and recovery is generally no longer possible. Understanding the importance of this time window is critical for healthcare providers in making decisions about resuscitation, brain death diagnosis, and potential organ donation.
The determination of brain death is complex and involves both scientific understanding and ethical considerations. As medical technology continues to advance, new methods of preserving brain function and improving the chances of recovery after cardiac arrest may emerge. However, the 6-12 minute barrier remains an essential threshold in the context of brain death, highlighting the importance of early and effective intervention in preventing irreversible brain injury.